Healthy Gums
Gum Disease Bone-Loss
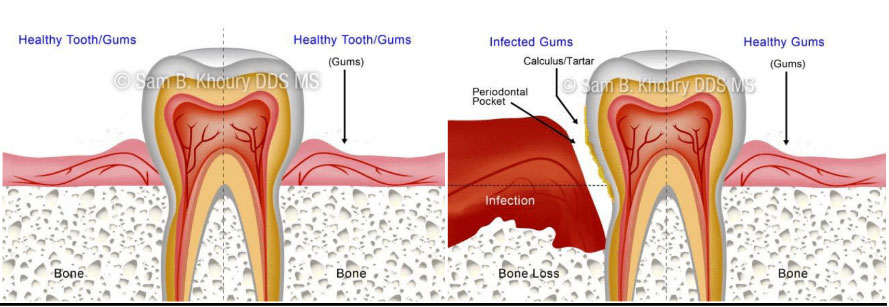
The term “periodontal” means “around the tooth.” Periodontal disease (also known as periodontitis and gum disease) is a common inflammatory condition which affects the supporting and surrounding soft tissues of the tooth; also the jawbone itself when in its most advanced stages.
Periodontal disease is most often preceded by gingivitis which is a bacterial infection of the gum tissue. A bacterial infection affects the gums when the toxins contained in plaque begin to irritate and inflame the gum tissues. Once this bacterial infection colonizes in the gum pockets between the teeth, it becomes much more difficult to remove and treat. Periodontal disease is a progressive condition that eventually leads to the destruction of the connective tissue and jawbone. If left untreated, it can lead to shifting teeth, loose teeth and eventually tooth loss. Periodontal disease is the leading cause of tooth loss among adults in the developed world and should always be promptly treated.
When left untreated, gingivitis (mild gum inflammation) can spread to below the gum line. When the gums become irritated by the toxins contained in plaque, a chronic inflammatory response causes the body to break down and destroy its own bone and soft tissue. There may be little or no symptoms as periodontal disease causes the teeth to separate from the infected gum tissue. Deepening pockets between the gums and teeth are generally indicative that soft tissue and bone is being destroyed by periodontal disease.
Here are some of the most common types of periodontal disease:
Aggressive Periodontitis– This form of gum disease occurs in an otherwise clinically healthy individual. It is characterized by rapid loss of gum attachment, chronic bone destruction and familial aggregation. Specific aggressive kind of bacteria has also been implicated in this disease.
Treatment: The treatment for aggressive periodontal disease are the same as those for chronic periodontal disease, but aggressive periodontal disease sufferers are far more likely to require a surgical intervention. This form of the disease is harder to halt and treat, but the dentist will perform scaling, root planing, antimicrobial, and in some cases laser procedures in an attempt to save valuable tissue and bone.
Chronic Periodontitis– Inflammation within supporting tissues cause deep pockets and gum recession. It may appear the teeth are lengthening, but in actuality, the gums (gingiva) are receding. This is the most common form of periodontal disease and occurs much more frequently in people over 45. It is characterized by progressive loss of attachment, interspersed with periods of rapid progression.
Treatment: Unfortunately unlike gingivitis, chronic periodontal disease cannot be completely cured because the supportive tissue cannot be rebuilt. However, the dentist can halt the progression of the disease using scaling and root planing procedures in combination with antimicrobial treatments. If necessary, the periodontist can perform surgical treatments such as pocket reduction surgery and also tissue grafts to strengthen the bone and improve the aesthetic appearance of the oral cavity.
Necrotizing Periodontitis- This form of the disease rapidly worsens, and often occurs in individuals suffering from systemic conditions such as HIV, immunosuppression and malnutrition. Necrosis (tissue death) occurs in the periodontal ligament, alveolar bone and gingival tissues.
Treatment: Necrotizing periodontal disease is extremely rare. Because it may be associated with HIV or another serious medical condition, it is likely the dentist will consult with a physician before commencing treatment. Scaling, root planing, antibiotic pills, medicated mouth wash and fungicidal medicines are generally used to treat this form of the disease.
Periodontitis Caused by Systemic Disease– Periodontal disease can be a symptom of a disease or condition affecting the rest of the body, and often begins at an early age. Medical conditions such as respiratory disease, diabetes and heart disease are common cofactors. The disease can behave like aggressive periodontal disease, working quickly to destroy tissue.
Treatment:Initially, the medical condition which caused the onset of periodontal disease must be controlled. The dentist will halt the progression of the disease using the same treatments used for controlling aggressive and chronic periodontal disease.
It is extremely important to note that periodontal disease can progress without any signs or symptoms such as pain. This is why regular dental checkups are exceptionally important. Described below are some of the most common signs and symptoms of periodontitis. If you have any of these signs or symptoms, the advice of a general dentist or periodontist should be sought as soon as possible: Unexplained bleeding – Bleeding when brushing, flossing or eating food is one of the most common symptoms of a periodontal infection. The toxins in plaque cause a bacterial infection which makes the tissues prone to bleeding.
Pain, redness or swelling– A periodontal infection may be present if the gums are swollen, red or painful for no apparent reason. It is essential to halt the progression of the infection before the gum tissue and jaw bone have been affected. It is also critical to treat the infection before it is carried into the bloodstream to other areas of the body.
Longer-looking teeth– Periodontal disease can lead to gum recession. The toxins produced by bacteria can destroy the supporting tissue and bones, thus making the teeth look longer and the smile appear more “toothy.”
Bad breath/halitosis–Although breath odor can originate from back of the tongue, the lungs and stomach, from the food we consume, or from tobacco use, bad breath may be caused by old food particles which sit between the teeth and underneath the gumline. The deeper gum pockets are able to house more debris and bacteria, causing a foul odor.
Loose teeth/change in bite pattern– A sign of rapidly progressing periodontitis is the loosening or shifting of the teeth in the affected area. As the bone tissue gets destroyed, teeth that were once firmly attached to the jawbone become loose or may shift in position.
Pus– Pus oozing from between the teeth is a definitive sign that a periodontal infection is in progress. The pus is a result of the body trying to fight the bacterial infection.
There are genetic and environmental factors involved in the onset of gum disease, and in many cases the risk of developing periodontitis can be significantly lowered by taking preventative measures.
Here are some of the most common causes of gum disease:
Poor dental hygiene– Preventing dental disease starts at home with good oral hygiene and a balanced diet. Prevention also includes regular dental visits which include exams, cleanings, and x-rays. A combination of excellent home care and professional dental care will ensure and preserve the natural dentition and supporting bony structures. When bacteria and calculus (tartar) are not removed, the gums and bone around the teeth become affected by bacteria toxins and can cause gingivitis or periodontitis, which can lead to tooth loss.
Tobacco use– Research has indicated that smoking and tobacco use is one of the most significant factors in the development and progression of gum disease. In addition to smokers experiencing a slower recovery and healing rate, smokers are far more likely to suffer from calculus (tartar) build up on teeth, deep pockets in the gingival tissue and significant bone loss.
Genetic predisposition– Despite practicing rigorous oral hygiene routines, as much as 30% of the population may have a strong genetic predisposition to gum disease. These individuals are six times more likely to develop periodontal disease than individuals with no genetic predisposition. Genetic tests can be used to determine susceptibility and early intervention can be performed to keep the oral cavity healthy.
Pregnancy and menopause– During pregnancy, regular brushing and flossing is critical. Hormonal changes experienced by the body can cause the gum tissue to become more sensitive, rendering them more susceptible to gum disease.
Chronic stress and poor diet– Stress lowers the ability of the immune system to fight off disease, which means bacterial infections may possibly beat the body’s defense system. Poor diet or malnutrition can also lower the body’s ability to fight periodontal infections, as well as negatively affecting the health of the gums.
Diabetes and underlying medical issues– Many medical conditions can intensify or accelerate the onset and progression of gum disease including respiratory disease, heart disease, arthritis and osteoporosis. Diabetes hinders the body’s ability to utilize insulin which makes the bacterial infection in the gums more difficult to control and cure.
Grinding teeth– The clenching or grinding of the teeth can significantly damage the supporting tissue surrounding the teeth. Grinding one’s teeth is usually associated with a “bad bite”or the misalignment of the teeth. When an individual is suffering from gum disease, the additional destruction of gingival tissue due to grinding can accelerate the progression of the disease
Medications – Many drugs including oral contraceptive pills, heart medicines, anti-depressants and steroids affect the overall condition of teeth and gums; making them more susceptible to gum disease. Steroid use promotes gingival overgrowth, which makes swelling more commonplace and allows bacteria to colonize more readily in the gum tissue.
Research studies have shown that there is a strong association between periodontal disease and other chronic conditions such as diabetes, heart disease, pregnancy complications and respiratory disease.Periodontal disease is characterized by chronic inflammation of the gum tissue, periodontal infection below the gum line and a presence of disease-causing bacteria in the oral region. Halting the progression of periodontal disease and maintaining excellent standards of oral hygiene will not only reduce the risk of gum disease and bone loss, but also reduce the chances of developing other serious illnesses. Common cofactors associated with periodontal disease:
Diabetes
A research study has shown that individuals with pre-existing diabetic conditions are more likely to either have, or be more susceptible to periodontal disease. Periodontal disease can increase blood sugar levels which makes controlling the amount of glucose in the blood difficult. This factor alone can increase the risk of serious diabetic complications. Conversely, diabetes thickens blood vessels and therefore makes it harder for the mouth to rid itself of excess sugar. Excess sugar in the mouth creates a breeding ground for the types of oral bacteria that cause gum disease.
Heart Disease
There are several theories which explain the link between heart disease and periodontitis. One such theory is that the oral bacteria strains which exacerbate periodontal disease attach themselves to the coronary arteries when they enter the bloodstream. This in turn contributes to both blood clot formation and the narrowing of the coronary arteries, possibly leading to a heart attack.
A second possibility is that the inflammation caused by periodontal disease causes a significant plaque buildup. This can swell the arteries and worsen pre-existing heart conditions. An article published by the American Academy of Periodontology suggests that patients whose bodies react to periodontal bacteria have an increased risk of developing heart disease. Pregnancy Complications
Women in general are at increased risk of developing periodontal disease because of hormone fluctuations that occur during puberty, pregnancy and menopause. Research suggests that pregnant women suffering from periodontal disease are more at risk of preeclampsia and delivering underweight, premature babies.
Periodontitis increases levels of prostaglandin, which is one of the labor-inducing chemicals. Elevated levels prostaglandin may trigger premature labor, and increase the chances of delivering an underweight baby. Periodontal disease also elevates C-reactive proteins (which have previously been linked to heart disease). Heightened levels of these proteins can amplify the inflammatory response of the body and increase the chances of preeclampsia and low birth weight babies.
Respiratory Disease
Oral bacterium linked with gum disease has been shown to possibly cause or worsen conditions such as emphysema, pneumonia and Chronic Obstructive Pulmonary Disease (COPD). Oral bacteria can be drawn into the lower respiratory tract during the course of normal inhalation and colonize; causing bacterial infections. Studies have shown that the repeated infections which characterize COPD may be linked with periodontitis.
In addition to the bacterial risk, inflammation in gum tissue can lead to severe inflammation in the lining of the lungs, which aggravates pneumonia. Individuals who suffer from chronic or persistent respiratory issues generally have low immunity. This means that bacteria can readily colonize beneath the gum line unchallenged by body’s immune system.
It is well documented that people who suffer from diabetes are more susceptible to developing infections than non-diabetes sufferers. It is not widely known that t periodontal disease is often considered the sixth complication of diabetes; particularly when the diabetes is not under proper control.
Periodontal disease (often called periodontitis and gum disease) is a progressive condition that often leads to tooth loss if treatment is not promptly sought. Periodontal disease begins with a bacterial infection in the gingival tissue which surrounds the teeth. As the bacteria colonize, the gum pockets become deeper, the gums recede as tissue is destroyed and the periodontitis eventually attacks the underlying bone tissue.
Diabetes is characterized by too much glucose (or sugar) in the blood. Type II diabetics are unable to regulate insulin levels which means excess glucose stays in the blood. Type I diabetics do not produce any insulin at all. Diabetes is a serious condition which can lead to heart disease and stroke.
Reasons for the Connection
Experts suggest the relationship between diabetes and periodontal disease can worsen both conditions if either condition is not properly controlled.
Here are ways in which diabetes and periodontal disease are linked:
Increased blood sugar – Moderate and severe periodontal disease elevates sugar levels in the body, increasing the amount of time the body has to function with high blood sugar. This is why diabetics with periodontitis have difficulty keeping control of their blood sugar. In addition, the higher sugar levels found in the mouth of diabetics provide food for the very bacteria that worsen periodontal infections.
Blood vessel thickening – The thickening of the blood vessels is one of the other major concerns for diabetes sufferers. The blood vessels normally serve a vital function for tissues by delivering nutrients and removing waste products. With diabetes, the blood vessels become too thick for these exchanges to occur. This means that harmful waste is left in the mouth and can weaken the resistance of gum tissue, which can lead to infection and gum disease.
Smoking – Tobacco use does a great deal of damage in the oral region. Not only does tobacco use slow the healing process, it also vastly increases the chances of an individual developing periodontal disease. For diabetics who smoke, the risk is exponentially greater. In fact, diabetic smokers aged 45 and over are twenty times more likely to develop periodontal disease.
Poor oral hygiene – It is essential for diabetics to maintain excellent levels of oral health. When daily brushing and flossing does not occur, the harmful oral bacteria can ingest the excess sugar between the teeth and colonize more freely below the gum line. This exacerbates the metabolic problems that diabetes sufferers experience.
Diagnosis and Treatment
It is of paramount importance for people suffering from any type of diabetes to see the dentist at least twice yearly for checkups and professional cleanings. Studies have shown that simple non-surgical periodontal treatments can lower the HbA1c (hemoglobin molecule blood test) count by as much as 20% in a six month period.
The dentist will use medical history, family history and dental X-rays to assess the risk factors for periodontal disease and determine the exact condition of the gums, teeth and underlying jawbone. If necessary the dentist will work in conjunction with other doctors to ensure that both the diabetes and the gum disease are being managed and controlled as effectively as possible
Non-surgical procedures performed by the dentist and dental hygienist include deep scaling, where calculus (tartar) will be removed from the teeth above and below the gumline, and root planing, where the root of the tooth is smoothed down to eliminate any remaining bacteria. Antibiotics may be applied to the gum pockets to promote healing.
Before and after periodontal treatment, the dentist and hygienist will recommend proper home care and oral maintenance as well as prescribing prescription mouthwashes which serve to deter further bacteria colonization
Periodontal disease, heart disease and stroke may seem to be unlikely bedfellows, but researchers have found that gum disease sufferers are nearly twice as likely to also suffer from coronary heart disease. In addition, research studies have discovered that oral infection is indeed a risk factor for stroke. People diagnosed with acute cerebrovascular ischemia were more likely to also be experiencing some degree of periodontal disease.
Periodontal disease is a progressive condition in which the gingival tissue surrounding the teeth is infected by the colonization of bacteria. Bacteria found in plaque colonize first above, then below the g gumline causing the tissue to pull away from the teeth. If periodontal disease is left untreated, deep pockets form between the gums and the teeth and the tissue of the underlying jawbone is also destroyed. The destruction of bone tissue causes the teeth to shift, wobble or completely detach from the bone.
Coronary heart disease occurs when the walls of the coronary arteries become progressively thicker due to the buildup of fatty proteins. The heart then suffers from a lack of oxygen and must labor significantly harder to pump blood to the rest of the body. Coronary heart disease sufferers sometimes experience blood clots which obstruct normal blood flow and reduce the amount of vital nutrients and oxygen the heart needs to function properly. This phenomenon often leads to heart attacks.
Reasons for the Connection
There is little doubt that the presence of periodontal disease can exacerbate existing heart conditions. The periodontist and cardiologist generally work as a team in order to treat individuals experiencing both conditions.
There are several theories which may explain the link between heart disease, stroke and periodontal disease, which include the following:
- Oral bacteria affect the heart – There are many different strains of periodontal bacteria. Researchers assert that some of these strains of bacteria enter the bloodstream and attach to the fatty plaques in the heart blood vessels (coronary arteries). This attachment then contributes to clot formation causing grave danger to the individual
- Inflammation – Periodontal disease causes severe inflammation in the gum tissue which elevates the white blood cell count and also the high sensitivity C-reactive protein levels. Research studies have shown that elevated levels of C-reactive proteins have been linked to heart disease.
- Infectious susceptibility –Individuals who experience particularly high levels of oral bacteria may have weaker immune systems and an inadequate host inflammatory response. These factors may induce specific vascular effects which have previously been shown to contribute in the onset of certain forms of heart disease.
Diagnosis and Treatment
Since periodontal disease appears to be a risk factor for both heart attack and stroke, it is extremely important to seek immediate treatment. Initially, the periodontist will conduct thorough examinations to assess the exact condition of the teeth, gums and jawbone. X-rays can be helpful in determining whether bone loss is prevalent in the upper and lower jaw.
The dentist is able to conduct deep cleaning treatments such as scaling and root planing to remove hardened calculus (tartar) deposits from the gum pockets. An antibiotic may be prescribed to ensure that the bacterium is completely destroyed and the periodontal infection does not spread. In most cases, periodontal disease can be prevented with regular cleanings and proper home care.
Researchers have shown that periodontal disease in expectant mothers actually exposes their unborn child to many different risks; particularly if they also happen to be diabetes sufferers.
Periodontal disease generally begins with a bacterial infection in the gum (gingival) tissue, which progressively destroys the tissue and the underlying bone. If left untreated, the bacterial infection causes an inflammatory reaction in the body, which can significantly deepen the gum pockets (space between the teeth and gums) and forces the gum and jawbone to recede.
Eventually, the progressive nature of periodontal disease causes the teeth to become loose and unstable, and eventually fall out.
Pregnancy causes many hormonal changes which increase the risk of the expectant mother to develop gingivitis (inflammation of the gum tissue) and periodontal disease. These oral problems have been linked in many research studies to preeclampsia, low birth weight of the baby and premature birth. Expectant women should seek immediate treatment for periodontal disease in order to reduce the risk of pre-natal and post-natal complications.
Reasons for the Connection
There are many different reasons why periodontal disease may affect the health of the mother and her unborn child:
- Prostaglandin Prostaglandin – Periodontal disease appears to elevate levels of prostaglandin in mothers who are suffering from the more advanced forms of the condition. Prostaglandin is a labor-inducing compound found in one of the oral bacteria strains associated with periodontitis. Elevated levels of prostaglandin can cause the mother to give birth prematurely and deliver a baby with a low birth weight.
- C – reactive protein (CRP) – This protein, which has been previously linked to heart disease, has now been associated with adverse pregnancy outcomes including preeclampsia and premature birth. Periodontal infections elevate C-reactive protein levels and amplify the body’s natural inflammatory response. Periodontal bacteria may enter the bloodstream causing the liver to produce CRP which leads to inflamed arteries as well as possible blood clots. These inflammatory effects can then lead to blocked arteries causing strokes or heart attacks.
- Bacteria spread –The bacteria which colonize in the gum pockets can readily travel through the bloodstream and affect other parts of the body. In pregnant women, research has found that oral bacteria and associated pathogens have colonized in the internal mammary glands and coronary arteries.
Diagnosis and Treatment
There are many safe, non surgical treatment options available for pregnant women. It is of paramount importance to halt the progress of periodontal disease in order to increase the chances of a safe and healthy delivery.
Initially, the dentist will assess the exact condition of the gums and jawbone in order to make a precise diagnosis. Scaling and root planing are two common non-surgical procedures used to rid the tooth-root surfaces of calculus (tartar) and remove the bacterial toxins from the gum pockets.
The advantages to the pregnant woman are plentiful. The risks of pregnancy complications caused by periodontal disease are reduced by as much as 50%, and these treatments will alleviate many unpleasant and harmful effects associated with gingivitis and periodontal infection.
Dentists can provide dental education and recommendations to the pregnant women on effective home care which can reduce risks that may affect her and/or her child’s health. Risks of periodontal disease can be vastly reduced by proper home care, smoking cessation, dietary changes and the ingestion of supplementary vitamins.
If you are a smoker who is concerned about the effects smoking can have on your health, congratulations! By accessing information about the negative impacts of tobacco use, you are taking the first step toward quitting.
Recent studies have shown that tobacco use may be one of the most significant risk factors in the development and progression of periodontal disease. In addition, following periodontal treatment or any type of oral surgery, the chemicals in tobacco can slow down the healing process and make the treatment results less predictable.
How Does smoking increase your risk for Periodontal Disease?
As a smoker, you are more likely than nonsmokers to have the following problems:
- Calculus Tartar– plaque that hardens on your teeth and can only be removed during a professional cleaning
- Deep pockets- between your teeth and gums
- Loss of the bone and tissue- that support your teeth If the calculus is not removed during a professional cleaning, and it remains below your gum line, the bacteria in the calculus can destroy your gum tissue and cause your gums to pull away from your teeth. When this happens, periodontal pockets form and fill with disease-causing bacteria. If left untreated, periodontal disease will progress. The pockets between your teeth and gums can grow deeper, allowing in more bacteria that destroy tissue and supporting bone. As a result, the gums may shrink away from the teeth making them look longer. Without treatment, your teeth may become loose, painful and even fall out.
Save Your Smile- Research shows that smokers loose more teeth than nonsmokers do. In fact, according to data from the Centers for Disease Control and Prevention, only about 20 percent of people over age 65 who have never smoked are toothless, while a whopping 41.3 percent of daily smokers over age 65 are toothless. In addition, research shows that current smokers don’t heal as well after periodontal treatment as former smokers or nonsmokers. But these effects are reversible if the smokers kick the habit before beginning treatment.
- Not Just Cigarettes- Other tobacco products are also harmful to your periodontal health. Smokeless tobacco also can cause gums to recede and increase the chance of losing the bone and fibers that hold your teeth in place. Pipe smokers also experience tooth loss at a rate similar to cigarette smokers.
- Other Oral Problems- Researches also have found that the following problems occur more often in people who use tobacco products:
- Oral cancer
- Bad breath
- Stained teeth
- Tooth loss
- Bone loss
- Loss of taste
- Less success with periodontal treatment
- Less success with dental implants
- Gum recession
- Mouth sores
- Facial wrinkling
Periodontal disease is characterized by a progressive loss of supportive gingival tissue in the gums and jawbone. It is the number one cause of tooth loss among adults in the developed world. Periodontal disease occurs when toxins found in oral plaque inflame and irritate the soft tissues surrounding the teeth. If left untreated, bacteria colonies initially cause the systematic destruction of gum tissue, and then proceed to destroy the underlying bone tissue.
Osteoporosis is a common metabolic bone disease which frequently occurs in postmenopausal women, and occurs less frequently in men. Osteoporosis is characterized by bone fragility, low bone mass and a decrease in bone mineral density. Many studies have explored and identified a connection between periodontal disease and osteoporosis.
A study conducted at the University of New York at Buffalo in 1995 concluded that post-menopausal women who suffered from osteoporosis were 86% more likely to also develop periodontal disease.
Reasons for the Connection
Though studies are still being conducted in order to further assess the extent of the relationship between osteoporosis and periodontal disease, the researchers have thus far made the following connections:
- Estrogen deficiency –Estrogen deficiency accompanies menopause and also speeds up the progression of oral bone loss. The lack of estrogen accelerates the rate of attachment loss (fibers and tissues which keep the teeth stable are destroyed).
- Low mineral bone density –This is thought to be one of several causes of osteoporosis, and the inflammation from periodontal disease makes weakened bones more prone to break down. This is why periodontitis can be more progressive in patients with osteoporosis.
Diagnosis and Treatment
Osteoporosis and periodontal disease are much less dangerous if they are diagnosed in the early stages. Once a diagnosis has been made, the dentist will generally work with the patient’s doctor to ensure that both diseases are effectively controlled.
Here are some methods commonly used to diagnose and treat the diseases:
- Routine dental x-rays – X-rays can be effectively used to screen for bone loss in the upper and lower jaw, and the dentist can provide interventions for preventing and treating periodontal disease. It is believed that minimizing periodontal disease will help treat osteoporosis.
- Estrogen supplements – Providing post-menopausal women with estrogen supplements lowers the rate of attachment loss and also lowers gingival inflammation, which in turn protects the teeth from periodontal disease.
- Assessment of risk factors – Dentists and doctors are able to closely monitor the patients that are at an increased risk of developing both diseases by assessing family history, medical history, X-ray results, current medications and modifiable risk factors. Tobacco use, obesity, poor diet and estrogen deficiency can all be managed using a combination of education, support and prescription medications
