Dental Implant Basics
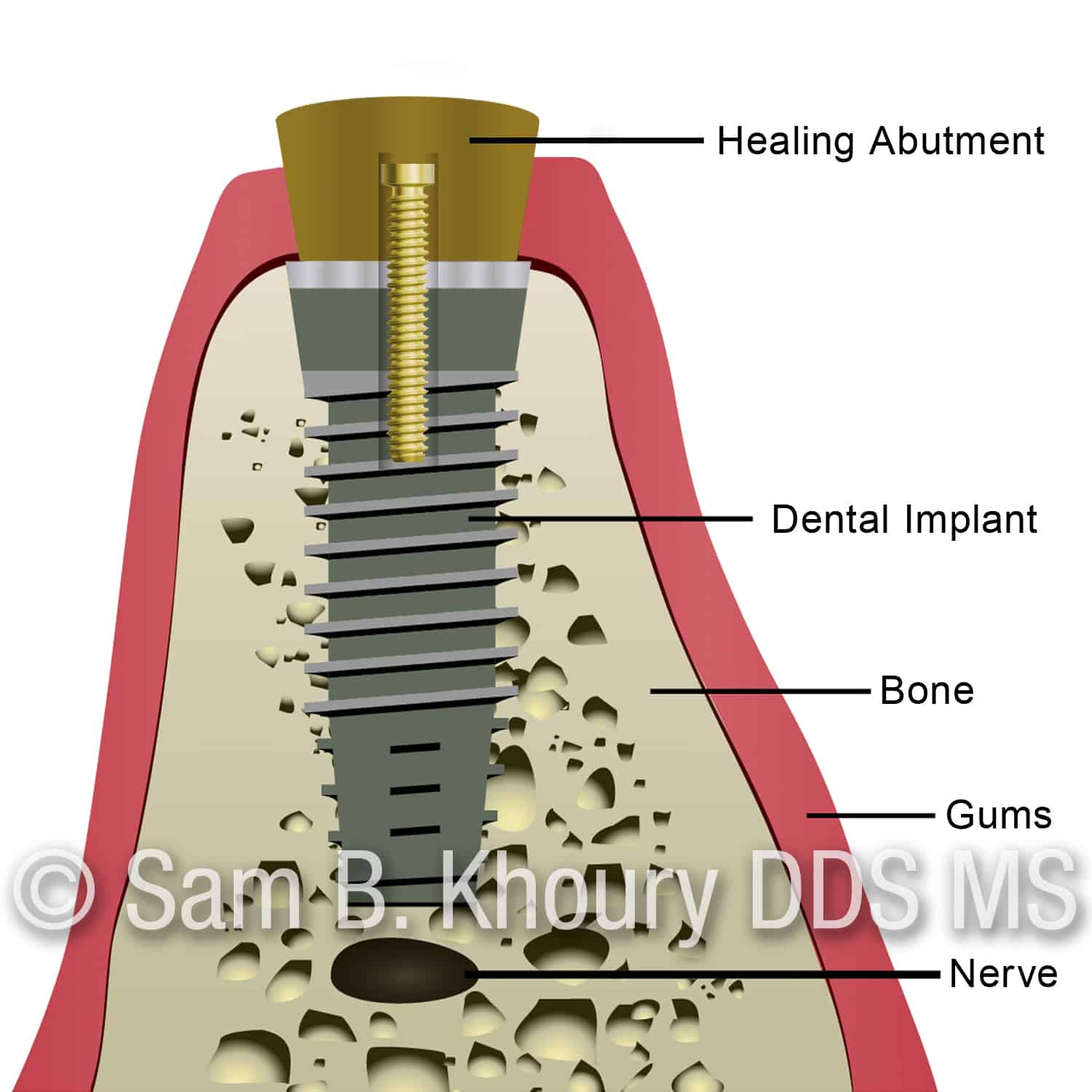
Dental Implant with a healing cover
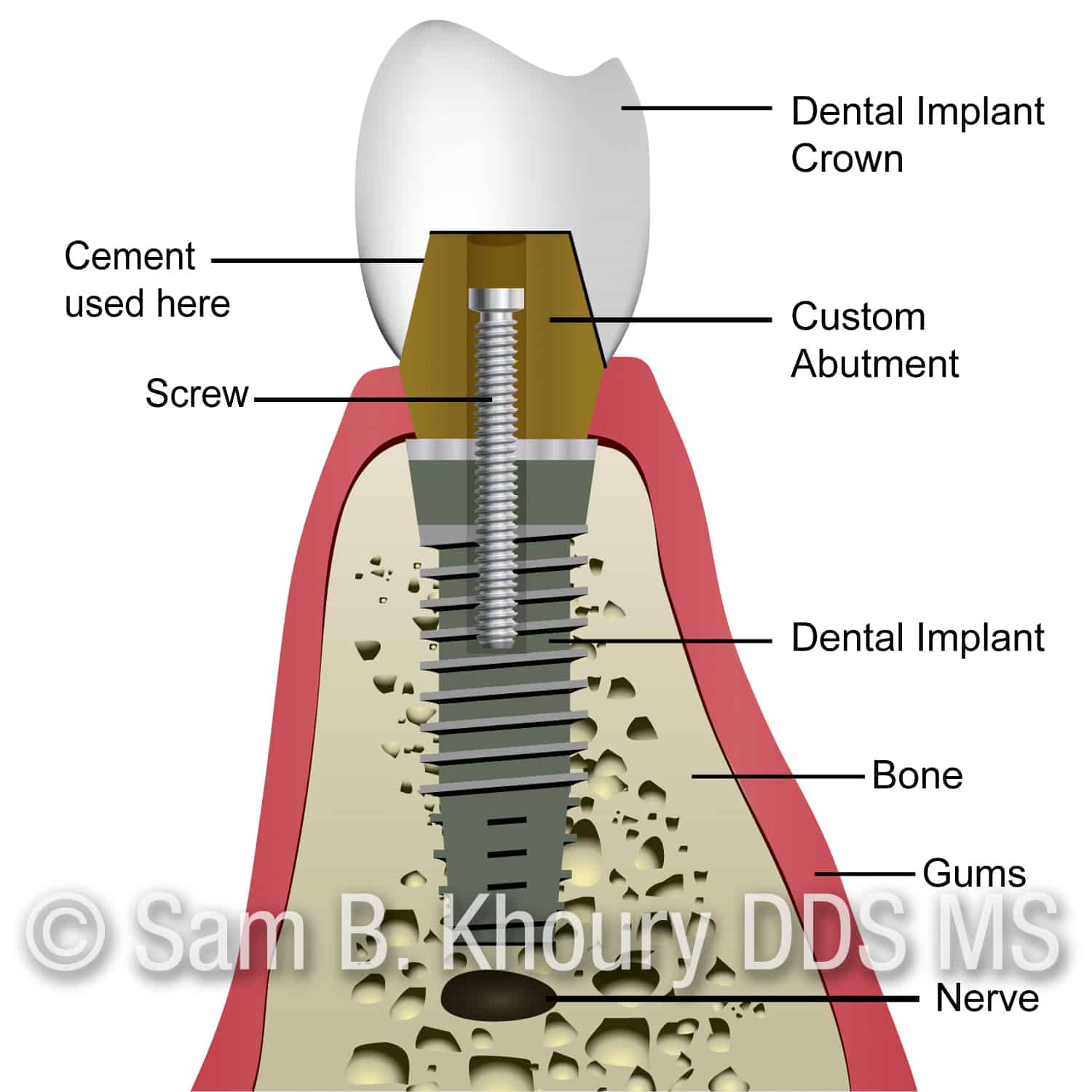
Complete dental implant with an abutment and a dental implant crown
Dental Implant with a healing cover
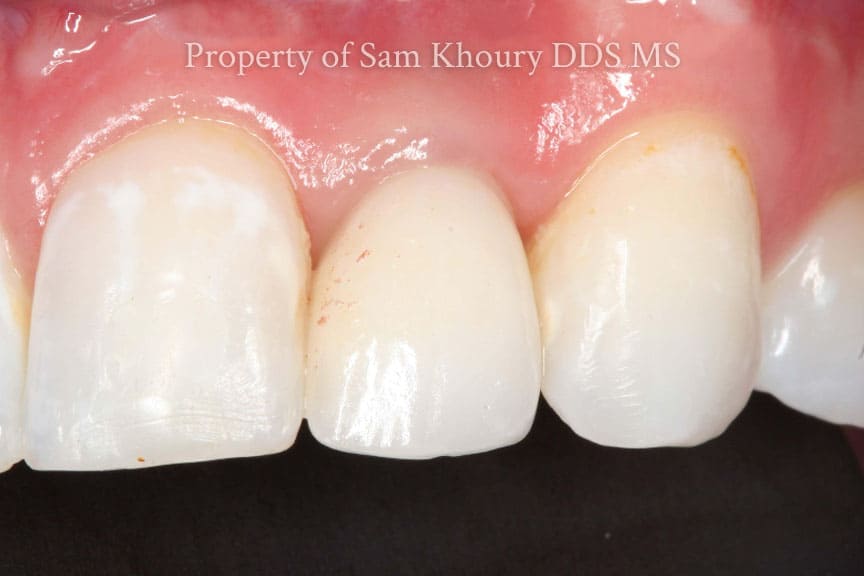
Complete dental implant with an abutment and a dental implant crown
Dental Implant with a healing cover
Complete dental implant with an abutment and a dental implant crown
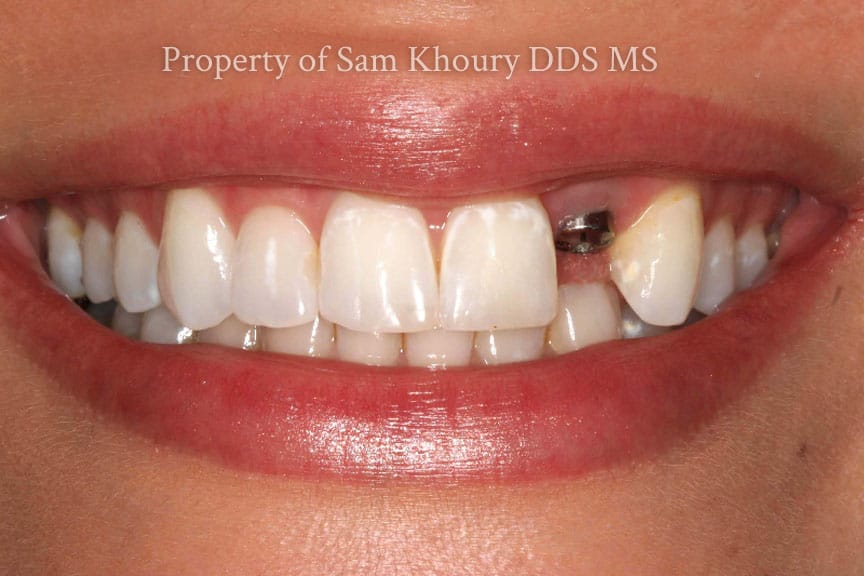
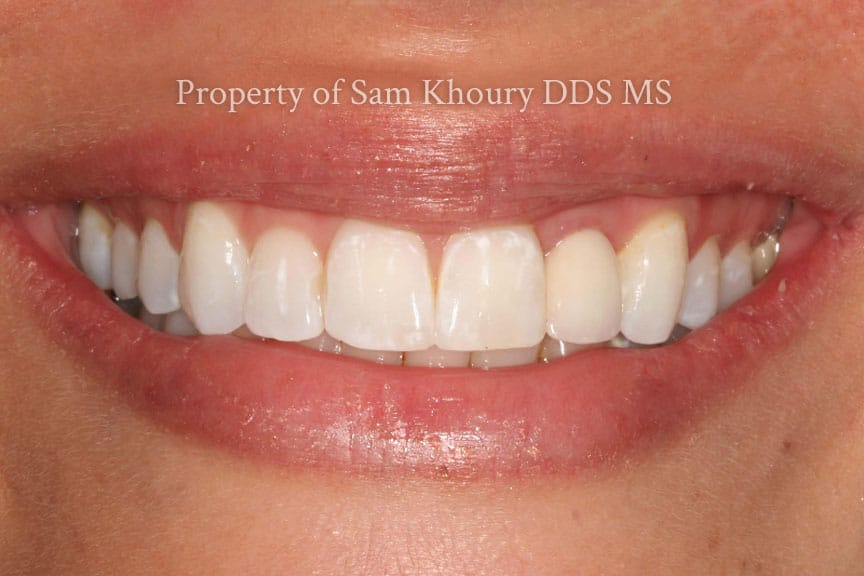
Dental implant surgery is a procedure that replaces a tooth root with a titanium metal, screw-like post that looks and functions much like a real tooth. The titanium in the implant fuses with your jawbone over a few months before an implant crown is made. The dental Implant is typically placed by the periodontist with a protective healing cap/abutment (Image 1). The dental implant final post (Custom Abutment) and the dental implant crown are typically made by the general dentist (Image 2)
In general, dental implants may be right for you if you:
- Have one or more missing teeth
- Have a jawbone that reached its full growth (Over 20 years old)
- Have adequate bone to secure the implants
- Have healthy oral tissues with no gum disease
- Do not have health conditions that may affect bone healing/li>
- Are unable or unwilling to wear dentures
- Want to improve your speech
- Are willing to commit several months to the process
Stages of Dental Implant Placement
Dental implant surgery is usually an outpatient procedure performed in stages, with healing time between procedures. The process of placing a dental implant involves multiple steps, including:
- Removal of the damaged tooth with bone (grafting) followed by 3-4 months of healing
- A dental 3D CT Scan (CBCT) is taken to check bone volume (Images 3, 4, 5)
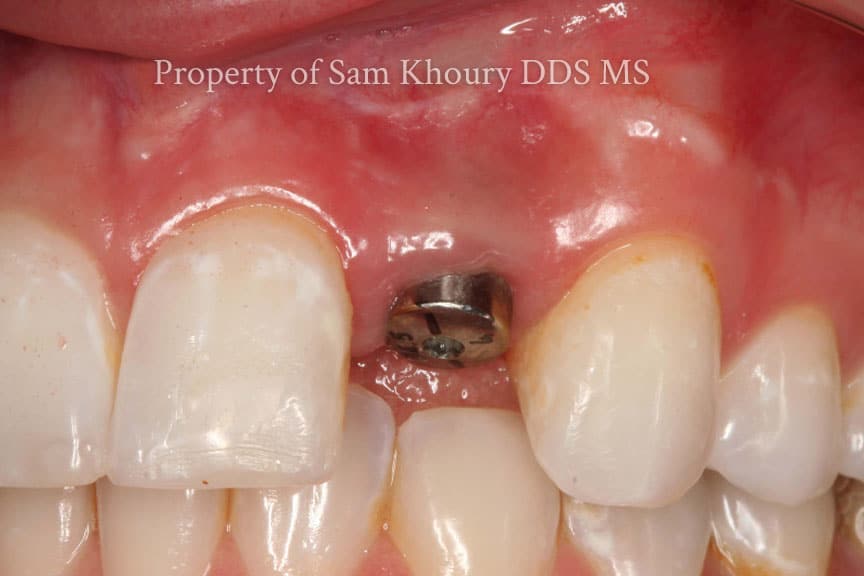
- Dental implant placement with a healing abutment (Image 1)
- Custom post/abutment and implant crown placement by the general dentist (See image 2)
What is the most important thing needed before dental implant surgery?
One of the most important requirements before dental implant surgery is the measurement of bone volume (height and width of the bone) as well as identifying any vital structures (nerves, and sinus location) using a Dental 3D CT scan (CBCT)g See Image 3. Using a CBCT is the Gold Standard for dental implant surgery. Planning a dental implant without this diagnostic 3D x ray is considered BELOW the standard of care.
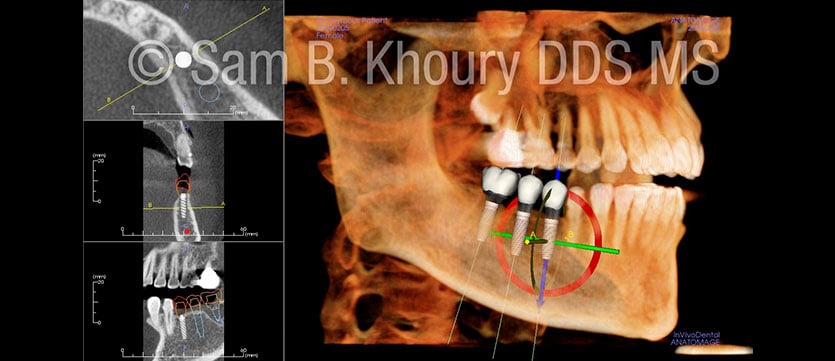
CBCT allows identification of narrow jawbone
(Image 4) which is not adequate for a dental implant vs wide jawbone which is what is needed for long-term success of the dental implant (Image 5)
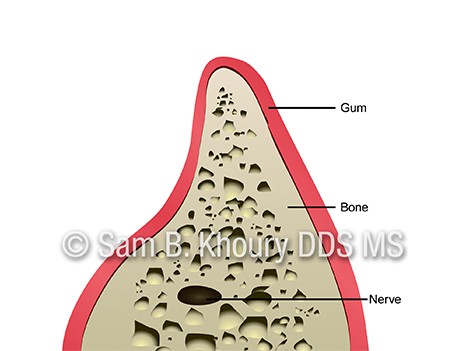
Narrow Jaw-Not good for dental implants
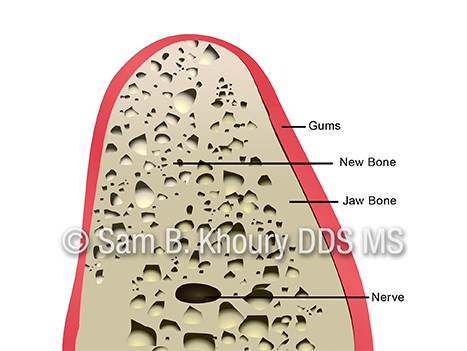
Wide Bone giving support for dental implants
Dental Implant Crown Designs
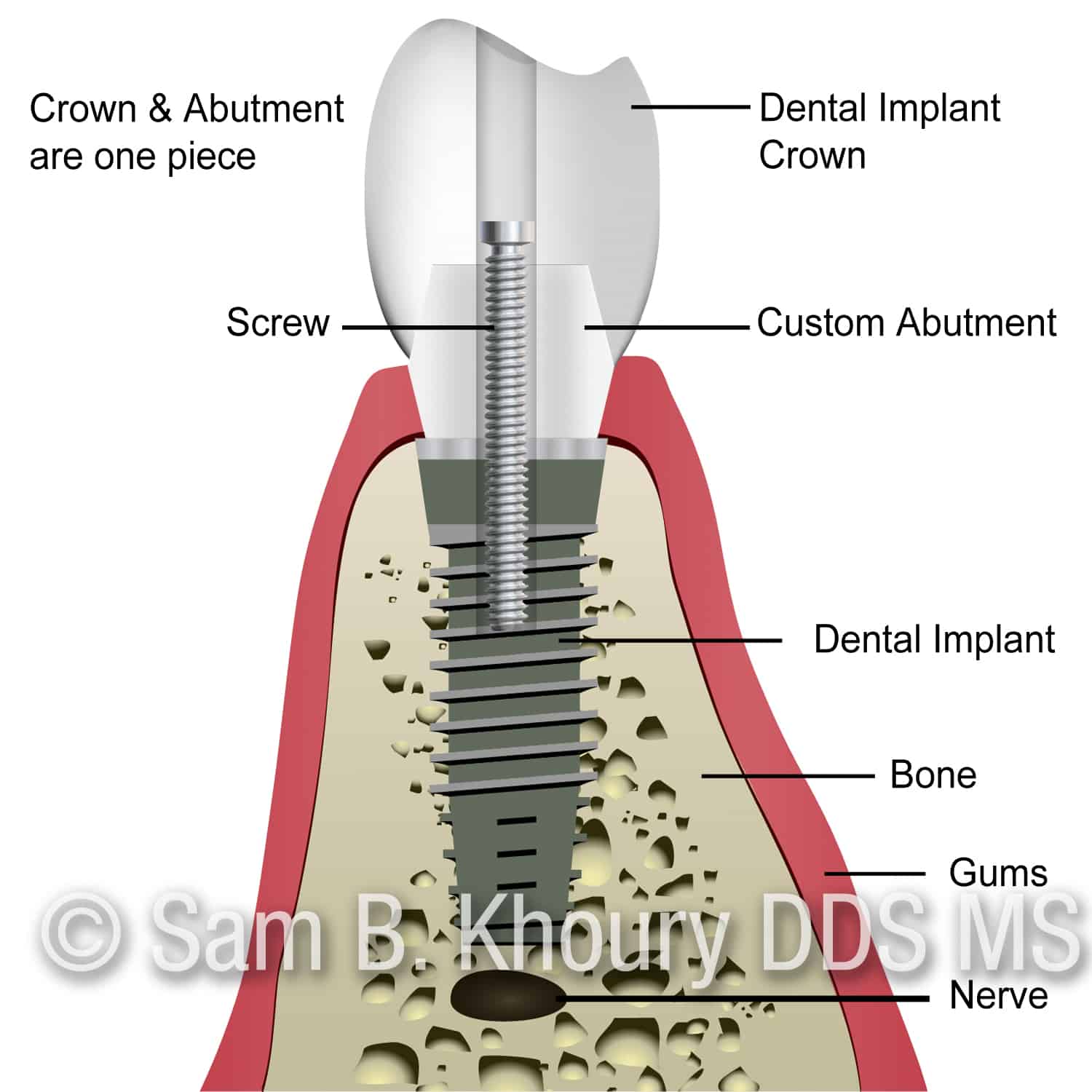
Screw retained Crown
A. Screw-Retained Crowns
The crown and the abutment are made together and are held together with one screw. The channel where the screw locks in, is typically closed with a white filling. The crown is not only recoverable, but no damage occurs upon removal of the crown. In the event of loosening or fracture, the crown can easily be removed. Cleaning, screw replacement and assessment of surrounding tissue is also possible. It may not always be possible to make screw-retained crown due to the angle of the implant especially in the front teeth.
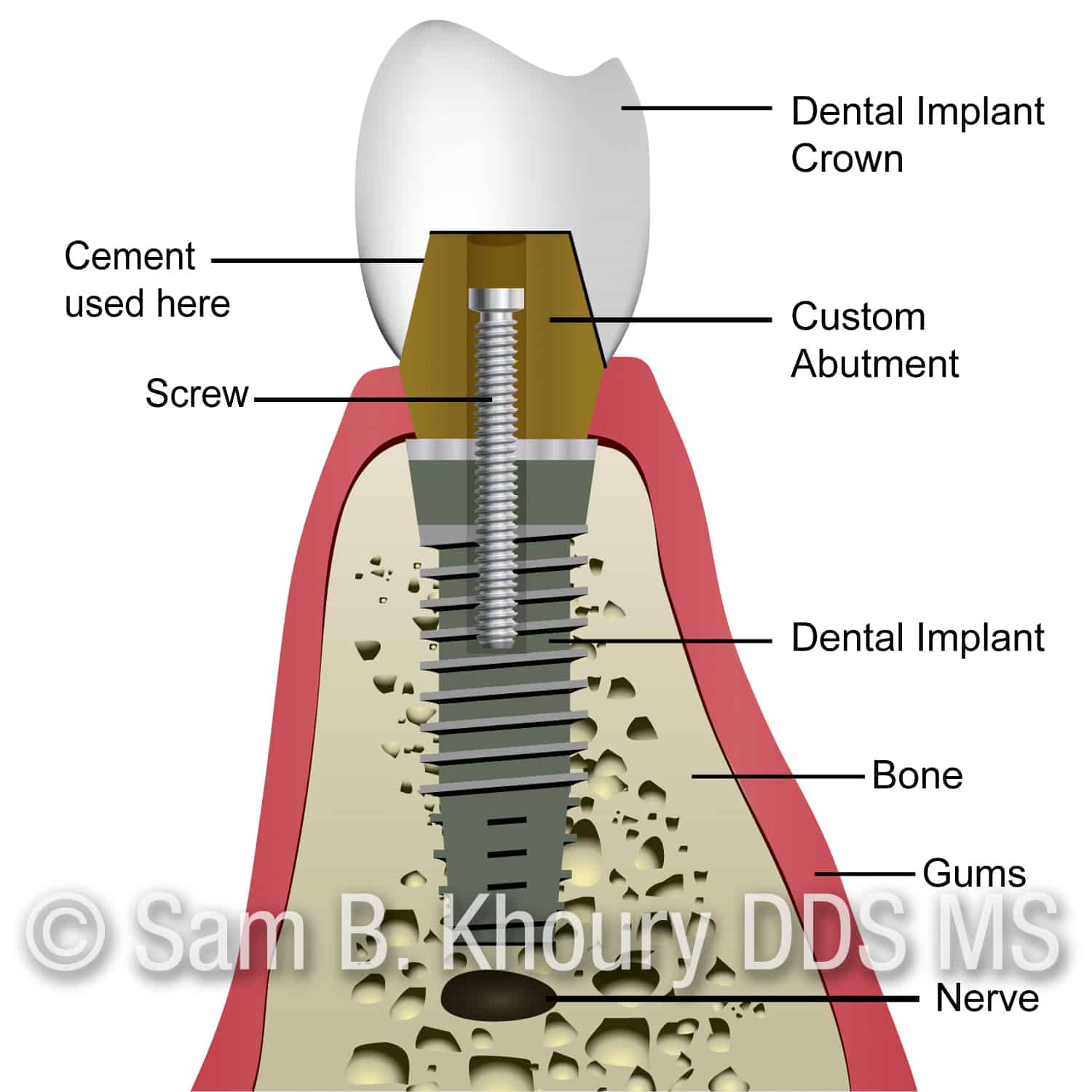
Cement retained implant Crown
B. Cement Retained Crowns
The crown and the abutment are made separately. The abutment is held together with a screw, and then the crown is typically cemented on top of the abutment. For cement-retained crowns, retrievability could be a major drawback. Cemented crowns may be recovered if the correct cement is used. While the screw-retained crown is certainly retrievable, removing a cement-retained crown can be a questionable undertaking if strong cements are used. Cement-retained restorations offer several advantages, including the elimination of unesthetic screw access holes and greater resistance to porcelain fracture. However, excess cement left behind inadvertently is a major problem and can result in soft tissue damage, bone loss and/or chronic inflammation.







